You might remember a while back that I posted about being part of a Diabetes Ireland delegation to attend a diabetes briefing for TD’s and Senators in Leinster House. My friends, Rebecca and Davina both gave powerful and emotional speeches to our audience about life with type 1 diabetes. I asked Rebecca if I could shared hers on Thriveabetes and she was game. Rebecca is also one of my partners in crime in organising Thriveabetes :-) Here are her words;

My name is Rebecca Flanagan, I live in Co. Clare and I have 3 daughters, the eldest of which has Type 1 Diabetes. She was diagnosed just before her 8th birthday and, at 16 years old now, has lived with this auto-immune condition for 8 years – a condition she will have for the rest of her life. This was the start of our whole family’s ‘new’ normal. This new normal for my daughter now involves a minimum of 4 finger prick blood sugar tests and a minimum of 4 insulin injections every day in order to stay alive. EVERY DAY!
Part of the new normal for our family was figuring out the insulin dose based on the amount of carbohydrates she would be eating, but it’s not a perfect science and so many variables can contribute to her care. Additional testing may be required for stressful times, like the students taking exams right now; anxiety, exercise, sickness. As parents we became our child’s nurse and doctor, hoping we had been given the proper training to keep our child healthy.
Time off work must be organized to attend hospital appointments, schools must be cooperative, and her siblings sometimes have to take a back seat. Middle of the night blood sugar tests often have to be done. There are times that the whole family becomes exhausted and burnt out.
But I know I’m not alone in this life with type 1 diabetes. There are about 3,000 families in Ireland trying to manage this balancing act with a type 1 child in Ireland. Some children are only babies at diagnosis – imagine trying to count the carbohydrates and a correct insulin dose for an infant, when it’s hard to tell how much even makes it past their mouth. Imagine trying to get a toddler to finish their dinner because they already had their insulin, and if they don’t they are in danger of having a hypo (or a low blood sugar, the consequences of which can lead to a coma or even death). Imagine having to come in to your child’s school every day at lunch, as I did, to administer their insulin injection because the school has no resources to support this. And then imagine hoping that they finished all of their lunch and maybe not run around TOO much at break, for fear of a hypo.
Now imagine the teenage years when they just don’t want to deal with it anymore – when they long to be like normal teenagers and not worry about testing all the time and taking insulin before having a quick ice cream with friends. Imagine their worries and fears for the future – my teenager shouldn’t have to worry about whether or not her life expectancy will be shortened, or complications like blindness or liver failure, or how difficult it might be to have a healthy pregnancy in the future.
These are all realities for families with type 1 children. Parents worry whether they are doing it all right whilst dealing with the public perception amongst those who just DON’T KNOW the difference between type 1 and type 2 diabetes. We are constantly defending and educating, constantly worrying. Worrying about complications, worrying about negative relationships with food (eating means testing means injecting), worrying about things like diabulimia – when teenagers stop taking their insulin in order to lose weight. There’s just so much worry.
There’s only so much that we, as parents, can do. We need the support of well trained and well-staffed clinical teams. Every family, regardless of location, should have quarterly hospital appointments with a paediatric endocrinologist, nurse specialist, dietician and psychological support service. Some children, my daughter included, are currently attending clinics with NO endocrinologist. Transitional clinics for teenagers which include psychological support are majorly needed.
The research has been completed. The Model of Care for all Children and Young People with Type 1 Diabetes was published in December 2015. It is time to get the funding in place to secure the basic medical staff requirements and get this system on track. The technologies available for the treatment of type 1 diabetes should also be available to all children – my daughter has lived with type 1 diabetes for 8 years and we are no closer to obtaining an insulin pump for her - they should be available to any family willing to put the work in.
Adequate staff and patient training now will reduce the long term impact on the health service by minimizing the potential for complications in adulthood. My daughter and all the other type 1 children will be using the health service for life, and we need up front support now so that they do not become a statistic of complications such as blindness and amputations.
I am asking for all the TDs in attendance today to please push for the Model of Care staff requirements to be filled and work towards all of the recommendations made in this document. The strategy is in place but the funding needs to follow NOW. Please support our families and push for funding to be utilised effectively. Our children did nothing to deserve this illness but they deserve adequate treatment and care from the health service on a nationwide level.
Thank you Rebecca for sharing your speech. And thanks to both Davina & Rebecca for explaining, so well, what living with type 1 diabetes is really like.
Our first request from our TD's was that 0.4% (€5m) of the health service's annual spend on diabetes (€1.3 billion this year) be re-directed towards funding the paediatric diabetes strategy, so that huge financial savings from preventing diabetes related complications would be accrued in future years.
But then! We asked for a multi-year health strategy with cross-party agreement for adults with diabetes. The National Programme for Diabetes Team have come up with this strategy but the need government to approve the funding to deliver this plan!
Diabetes is costing the government €1.3 billion this year and over €800 million of that will be spent on dealing with the complications of diabetes. We can reduce the amount spent on complications each year by directing the financial savings that the HSE has made, in the recent years by working with the diabetes community, in reducing the cost of diabetes medications and devices. We need those savings reallocated to providing the manpower resources to cope with the rising numbers and to encourage more effective daily management and better health outcomes.
So what's next? Well, we can try to use every opportunity to remind our TD's why we need this. We need it because those of us who do not have diabetic complications want to stay that way for as long as possible. We need support from our medical teams to maintain that journey. Those of us who already have complications need the support of a complete medical team to minimise the damage of those complications.


 On Wednesday 22 June in Leinster House,
On Wednesday 22 June in Leinster House, 
 Type 1 Diabetes
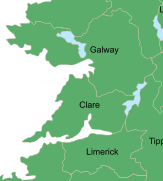
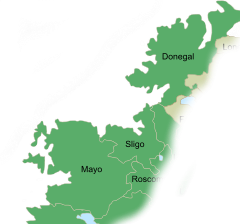
To implement the Paediatric Model of Care recently launched by the Minister for Health, to meet demand in Sligo, Donegal and Mayo, our children with type 1 diabetes need;
Type 1 Diabetes
To implement the Paediatric Model of Care recently launched by the Minister for Health, to meet demand in Sligo, Donegal and Mayo, our children with type 1 diabetes need; To implement the Paediatric Model of Care, recently launched by the Minister for Health, to meet demand in Cork & Kerry our children with type 1 diabetes need;
To implement the Paediatric Model of Care, recently launched by the Minister for Health, to meet demand in Cork & Kerry our children with type 1 diabetes need; Type 1 Diabetes
To implement the Paediatric Model of Care, recently launched by the Minister for Health, to meet demand in the HSE North East area and Dublin North our children with type 1 diabetes need;
Type 1 Diabetes
To implement the Paediatric Model of Care, recently launched by the Minister for Health, to meet demand in the HSE North East area and Dublin North our children with type 1 diabetes need; To implement the Paediatric Model of Care recently launched by the Minister for Health and to meet demand in the Our Lady’s Hospital, Crumlin, Wexford General Hospital and St Luke’s Hospital, Kilkenny, our children with type 1 diabetes need;
To implement the Paediatric Model of Care recently launched by the Minister for Health and to meet demand in the Our Lady’s Hospital, Crumlin, Wexford General Hospital and St Luke’s Hospital, Kilkenny, our children with type 1 diabetes need; Type 1 Diabetes
To implement the Paediatric Model of Care recently launched by the Minister for Health and to meet demand in AMNCH, Tallaght and the Midlands Regional Hospitals, our children with type 1 diabetes need;
Type 1 Diabetes
To implement the Paediatric Model of Care recently launched by the Minister for Health and to meet demand in AMNCH, Tallaght and the Midlands Regional Hospitals, our children with type 1 diabetes need;