 A few of you will have come across a FaceBook post in the Diabetes in Ireland Private Group from Debbie Davis who helps the Sunrise Foundation collect up unused and unneeded diabetes supplies such as old redundant glucose meters and test strips which are then send to underprivileged families with diabetes in Africa.
I wanted to find out a little more about the Sunrise Foundation and the work that they do, so Debbie very kindly put me in touch with Matilda Chongwa the CEO. Matilda has written this week’s blog post about her foundation.
A few of you will have come across a FaceBook post in the Diabetes in Ireland Private Group from Debbie Davis who helps the Sunrise Foundation collect up unused and unneeded diabetes supplies such as old redundant glucose meters and test strips which are then send to underprivileged families with diabetes in Africa.
I wanted to find out a little more about the Sunrise Foundation and the work that they do, so Debbie very kindly put me in touch with Matilda Chongwa the CEO. Matilda has written this week’s blog post about her foundation.
SUNRISE FOUNDATION INTERNATIONAL IRELAND.
What is the Sunrise Foundation?
My name is Matilda Chongwa. I am the CEO of Sunrise Foundation. 31 years ago, my mum was diagnosed with diabetes in Cameroon in a little village called Bali Nyonga in the North West Region of Cameroon. My siblings and I were all very young and did not know what diabetes was all about and the only thing we were told by my dad was that my mum was going to die because she was suffering from a sickness that she has to be on medication throughout her life. She was very ill and helpless in the hospital. She lost a lot of weight and she spent a whole year in the hospital. When she came out of the hospital she was always on medication and even now her life is all centred around medication and insulin.
With this in my mind, I was always thinking of ways to help my mum and others in the same situation. My mum was the first to be diagnosed with diabetes in the family and some of my aunties and uncles who were diagnosed after my mum died because they could not afford medication. Diabetes medication in Cameroon is very expensive and a lot of people cannot afford and they died on regular basis.
THE WORK OF THE SUNRISE FOUNDATION
When I came to Ireland I thought it was the right time for me to create awareness and support people with diabetes in Ireland and most especially in Africa where a lot of them are dying. The worse is that parent who cannot afford medication turn to invest on their health with the little they have and the children cannot afford education. Most children from families with diabetes cannot afford education so one of the things we do at Sunrise Foundation is education sponsorship for children from extremely poor families with diabetes in Africa.
 What we have achieved so far:
What we have achieved so far:
- We have successfully organised so many diabetes awareness events in Ireland. Where we get Irish medical doctors to talk about diabetes
- We donated €1,000 to Diabetes Ireland.
- We donated €400 to Diabetes Mater private.
- We have also celebrated World Diabetes Day in Ireland with a Fashion show {Fashion Against Diabetes}
- We have taken Irish Diabetes Consultants, doctors, and Sunrise volunteers to Africa for free screening and awareness on Diabetes and High Blood Pressure
- We have been featured on TV and newspapers in Ireland and Africa because of our work with the Sunrise Foundation.
- We have won 4 recognition awards from creating health awareness in Ireland and Africa.
- The CEO/Founder Matilda Chongwa was recognised last year in Germany As an African Living Legend for Diaspora Engagement International, through the African Living Legend Awards. All thanks to Sunrise Foundation Diabetes project.
 NEXT TRIP TO AFRICA
NEXT TRIP TO AFRICA
Our Next trip to Africa is in November and that is why Debbie Davies is collecting, medication, insulin, test trips and glucometers. I met Debbie Davies in 2015 with her daughter Caitlin Davis who had type 1 diabetes. She used to come to Diabetes awareness events organised by Sunrise Foundation and shared her life story about living with type 1 Diabetes and unfortunately, she died last year. She is greatly missed by The Sunrise Foundation Team and those she motivated with her stories and advice on how to live with Diabetes.
After her death, her lovely mother Debbie Davis decided to keep the relationship with Sunrise Foundation by organising collection of diabetes medication for Sunrise Foundation Diabetes project in Africa. We were in Nigeria in May for 12 days and all the collection were donated to St Mary's Hospital in Isolo, Nigeria. This donation was done in the presence of Dr Richard Firth who is a Diabetes Consultant in Mater Private who was the head doctor with us in Nigeria.
If you have items to donate to our next trip to Africa please contact Debbie via email davdebbie@gmail.com or Phone 085 2880489.
UPCOMING EVENT ORGANISED BY SUNRISE FOUNDATION VOLUNTEERS
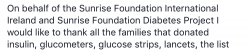
We are organising the World Diabetes Fashion Show on the 4th of November at the Hilton hotel, Dublin Airport on the Malahide road.
This event is organised by the Sunrise Foundation in partnership with the Diabetes Centre Mater Private Hospital. We would like to invite you all to come and share the day with other people with diabetes who will be sharing their stories and celebrating the World Diabetes Day. We are also looking for volunteers to travel with the team or who want to share their life story to help others.
Sunrise Foundation Contact Details:
- Matilda Chongwa
- Phone: 083 1644110
- Email: info@sunrisefoundation.ie
- Sunrise Foundation International Ireland Facebook Page
- Website http://sunrisefoundation.ie/
- Instagram is sunrise_foundation
- Supplies and Medical donations to: Debbie Davis davdebbie@gmail.com or 0752880489




